Top 10 Intramedullary Nail Techniques for Optimal Fracture Healing?
Intramedullary nails, often referred to as nail intramedullari, play a crucial role in orthopedic surgery. They are designed to stabilize fractures, ensuring proper alignment and healing. Surgeons utilize various techniques to enhance recovery and reduce complications.
Selecting the right technique is vital for optimal outcomes. Each method has its nuances, influencing patient recovery. For instance, the angle of insertion can affect stability. Patients should be aware that nail placement significantly impacts healing time.
Despite advancements, challenges persist in using Nail Intramedullari. Some patients may experience complications, leading to reflections on technique choices. Understanding these options can empower both surgeons and patients in the healing journey. Ultimately, the best approach should prioritize individual needs and circumstances.
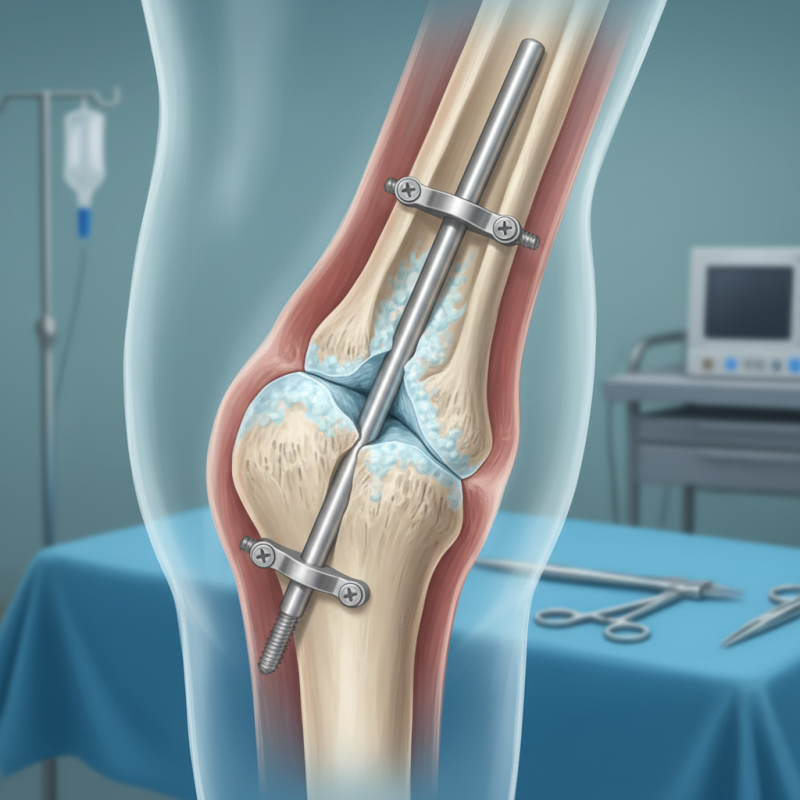
Table of Contents [Hide]
Introduction to Intramedullary Nail Techniques
Intramedullary nail techniques are essential in modern fracture management. These methods offer stable fixation and promote optimal healing. Surgeons often seek ways to enhance outcomes. The choice of nail type and insertion technique significantly impacts recovery.
Different factors can complicate the process. The anatomy of each patient varies. Additionally, the type and location of the fracture play a crucial role. Surgeons must assess soft tissue injuries and bone quality. Misalignment during insertion can lead to poor healing. This highlights the need for precision and skill.
While many techniques exist, challenges remain. Not all methods are suitable for every case. Surgeons may encounter difficulties in determining the best approach. Continuous education and practice are vital. Each procedure can serve as a learning opportunity. Reflection on past cases often leads to improvement.
Assessment of Fracture Types for Nail Selection
When it comes to selecting the right intramedullary nail for fracture healing, assessment of fracture types is critical. Different fracture patterns—like transverse, comminuted, and spiral—each require tailored approaches. Research from the Journal of Orthopaedic Trauma indicates that approximately 80% of long bone fractures are best treated with intramedullary nailing. However, the success rate varies based on injury classification.
Nails exhibit unique biomechanical properties. For instance, a comminuted fracture may require a nail that can provide rotational stability. Data shows that nails with enhanced interlocking capabilities can reduce the risk of malunion by nearly 40%. Despite this, clinicians often overlook fracture types in nail selection. This gap in decision-making can lead to prolonged recovery and complications.
Surgeons must remain vigilant. A recent survey found that 25% of orthopedic surgeons feel unprepared when selecting the right nail. This uncertainty reflects the need for better training and resources. Decisions should not be rushed, as each fracture presents distinct challenges. Using a systematic approach for assessment can significantly improve patient outcomes and enhance fracture healing success rates.
Preparation and Sterilization of Surgical Instruments
In surgical settings, the preparation and sterilization of instruments is crucial. Clean tools ensure patient safety and optimal healing. Every instrument must be checked for cleanliness before use. This includes removing any debris or bioburden. The sterile field should never be compromised.
Tips: Always use a compatible cleaning solution for your instruments. Pay attention to manufacturer recommendations. Consider using ultrasonic cleaners for thorough cleaning.
Sterilization follows cleaning. Autoclaving is a common method that uses high-pressure steam. Ensure the right temperature and timing. Instruments should be wrapped properly to maintain sterility. Improper wrapping could lead to contamination.
Tips: Regularly test the autoclave's efficiency. Biological indicators can confirm sterilization success. Always record sterilization cycles and maintain logs for accountability.
Step-by-Step Techniques for Nail Insertion
Intramedullary nail insertion is a common technique for fracture healing. Precise steps are critical for success. Begin by positioning the patient correctly. This enhances surgical visibility. The preferred entry point is often at the proximal end of the fracture site. The optimal angle of entry should be between 5-15 degrees to the medullary canal.
Once the skin is prepped and draped, use imaging to guide your incision. Accurate entry reduces risk. After making a small incision, you must carefully ream the canal. This step helps create a path for the nail. Studies show that the choice of reaming technique impacts recovery time. Full reaming can decrease complications. However, it may also prolong surgery duration.
After reaming, introduce the nail. Ensure it aligns with the fracture. Misalignment can hinder healing. Apply compression if required, making sure the hardware secures firmly. Monitor for complications like malunion or nonunion. Understanding common pitfalls can enhance outcomes. Each step requires reflection and adjustment for optimal healing. The balance of technique and patient-specific factors is vital.
Postoperative Care and Monitoring for Optimal Healing
Postoperative care is vital for fracture healing after intramedullary nail surgery. Patients often feel pain and discomfort. Managing these symptoms is essential. Pain relief should be tailored to individual needs. Regularly assess the effectiveness of prescribed medications. Adjustments might be necessary to enhance comfort levels.
Monitoring the surgical site is crucial. Patients should watch for signs of infection. Any redness, swelling, or unusual discharge requires immediate attention. Movement restrictions must be followed strictly. Physical therapy often starts early to prevent stiffness. But patients should avoid overstressing the healing bone.
Follow-up appointments are important. X-rays will help monitor healing progress. This process may take longer than expected. Patience is key, as not all cases will heal at the same pace. Regular check-ins can also provide psychological support. Overall, a focused approach to postoperative care can lead to better outcomes in recovery.
Top 10 Intramedullary Nail Techniques for Optimal Fracture Healing - Postoperative Care and Monitoring for Optimal Healing
| Technique | Indication | Postoperative Care | Monitoring | Healing Time |
|---|---|---|---|---|
| Locked Intramedullary Nailing | Diaphyseal fractures | Pain management, weight-bearing restrictions | Radiographic assessments | 6-12 weeks |
| Antegrade Nailing | Proximal femur fractures | Thromboembolic prophylaxis | Observe for complications | 8-16 weeks |
| Retrograde Nailing | Distal femur fractures | Physical therapy initiation | Follow-up imaging | 6-12 weeks |
| Interlocking Nailing | Complex fractures | Regular swelling assessment | Bone healing evaluations | 12-20 weeks |
| Bending Reinforcement | Osteoporotic fractures | Nutritional support | Monitor for nonunion | 10-14 weeks |
| Blocking Techniques | Torsional and bending stability issues | Rehabilitation exercises | Functionality tests | 8-16 weeks |
| Nail Slot Technique | Intramedullary fixations | Wound care | Assess mobility | 8-14 weeks |
| Submuscular Nailing | Humeral shaft fractures | Pain management protocols | Regular physiotherapy | 6-12 weeks |
| Bamboo Nailing | Pediatric fractures | Gentle mobilization | Visual assessments | 4-10 weeks |
| Sliding Nailing | Fractures with sliding tendencies | Activity modification | Biomechanical evaluation | 10-16 weeks |